Bipolar Disorder (BD)
Bipolar disorder is a common mood disorder that causes extreme shifts in mood, activity levels, and energy. There are three states that are typical of bipolar disorder: mania/hypomania (a ‘high’ state), depression (a ‘low’ state) and a normal state. The onset of bipolar disorder is usually between the ages of 15 and 30.
Overview
Symptoms
Diagnosis
Causes/Why Me?
Epidemiology
Treatment Approaches
What Can I Do For Myself?
Risk Factors
Comorbidities
Youth Specific Features
Summary
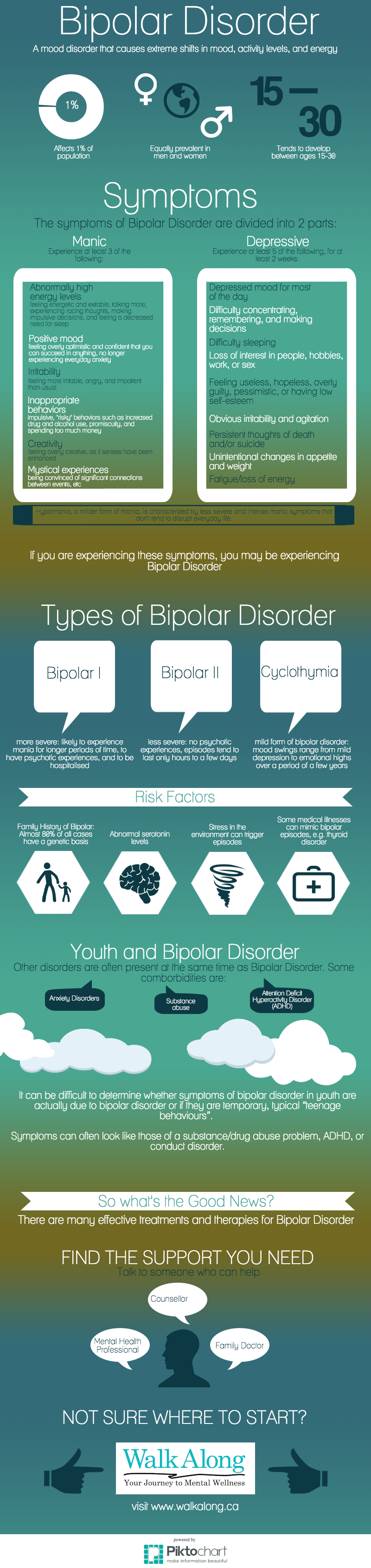
Infographic
Bipolar disorder is a common mood disorder that causes extreme shifts in mood, activity levels, and energy. There are three states that are typical of bipolar disorder: mania/hypomania (a ‘high’ state), depression (a ‘low’ state) and a normal state. The onset of bipolar disorder is usually between the ages of 15 and 30.
There are two main types of bipolar disorder: bipolar disorder I and bipolar disorder II. Bipolar disorder I is the more severe disorder, with individuals being more likely to experience mania for longer periods of time, to have psychotic experiences, and to be hospitalised. Bipolar disorder II is generally viewed as less severe, with no psychotic experiences, and with episodes tending to last only hours to a few days. Cyclothymic disorder is a mild form of bipolar disorder in which the mood swings range from mild depression to emotional highs over a period of a few years.
It is important to note that everyone has mood swings from time to time. It is only when these moods become extreme and interfere with personal and professional life that bipolar disorder may be present and medical assessment may be needed.
Mania
During a manic episode, a person will feel abnormally happy, optimistic and euphoric, or unusually angry, irritable, and disruptive for at least a week. If you are experiencing a manic episode, you will be experiencing at least 3 of these 6 symptoms:
- High energy levels: feeling abnormally energetic and exitable, talking more, experiencing racing thoughts, making impulsive decisions, and feeling a decreased need for sleep.
- Positive mood: feeling overly optimistic and confident that you can succeed in anything, and no longer experiencing everyday anxiety.
- Irritability: feeling more irritable, angry and impatient than usual.
- Inappropriate behaviors: can usually be seen through impulsive ‘risky’ actions such as increased use of alcohol and drugs, excessive spending of money, and getting into relationships that are later regretted.
- Creativity: feeling overly creative, “seeing things in a new light”, and feeling as if ones senses have been enhanced.
- Mystical Experiences: being convinced that there are significant connections between events, a higher frequency of coicidences, believing that things are of special importance, and feeling more connected with nature.
Click here to view the DSM-IV Diagnostic Criteria for a manic episode.
Hypomania
A hypomanic episode is characterized by similar symptoms as mania but of lesser severity and intensity, and lasts for at least 4 days. Hypomania tends to not disrupt one’s daily life in the way that manic episodes do, but must be treated so that it does not evolve into full-blown mania and depression. If you are experiencing a hypomanic episode, you will be experiencing at least 3 of the 6 symptoms described above.
Click here to view the DSM-IV Diagnostic Criteria for a hypomanic episode.
Major depressive episode
During a depressive episode, a person will feel abnormally sad or down to a degree that interferes with their ability to function in everyday life. At least 5 of these 9 symptoms must be present for at least two weeks:
- Depressed mood for most of the day
- Difficulty concentrating, remembering and making decisions
- Difficulty sleeping
- Loss of interest in people, hobbies, work, or sex
- Feeling useless, hopeless, overly guilty, pessimistic, or having low self-esteem
- Obvious irritability and agitation
- Persistent thoughts of death and/or suicide
- Unintentional changes in appetite and weight
- Fatigue/loss of energy
Click here to view the DSM-IV Diagnostic Criteria for a major depressive episode
Other symptoms
Sometimes, people with bipolar disorder will experience psychotic symptoms such as losing touch with reality (e.g.hearing voices, or having unrealistic ideas). Up to 25% of people with bipolar disorder also experience movement problems such as physical agitation or slowness. Some individuals with psychotic symptoms and movement difficulties may be wrongly diagnosed as having schizophrenia [Read More].
Cyclothymia
Cyclothymic disorder is a mild form of bipolar disorder in which the mood swings range from mild depression to emotional highs over a period of a few years.
It is characterized as episodes of hypomania and mild depression recurring consistently for over 2 years (1 year in children and adolescents). The mood swings are less severe than bipolar disorder and major depressive disorder [Read More].
To be diagnosed with Bipolar disorder I, one must be experience a manic episode for at least one week, and a depressive episode for at least two weeks.
To be diagnosed with Bipolar disorder II, one must experience a hypomanic episode for at least four days and a depressive episode for at least two weeks.
To be diagnosed with Cyclothymic disorder, a person must frequently switch between hypomanic and major depressive episodes for at least two years.
The symptoms must not be the result of another medical disorder such as thyroid disorder, vitamin B12 deficiency, adrenal disorder, or neurological disorder. Stimulant or steroid drug abuse and medications used as treatment for Parkinson’s Disease can also cause symptoms of mania, especially in people over 40 years of age.
Genetics
Bipolar disorder tends to run in families and a child with a parent or sibling with bipolar disorder is four to six times more likely to develop it than a child with no family history of bipolar. In 80% of bipolar cases, the cause has been linked to genetics.
Biological
Abnormal serotonin levels in the brain are also believed to be one of the causes of the extreme mood swings experienced by someone with bipolar disorder because of serotonin’s effect on other brain chemicals.
Environmental
Although stress is not a cause of bipolar disorder itself, a particularly stressful life event can trigger episodes in someone with the illness. Seasons may also play a role in the onset of bipolar disorder, with spring as the season with the highest chance of triggering a depressive or manic episode.
Medical illness
Some illnesses, such as thyroid disorder, adrenal disorder, vitamin B12 deficiency, and multiple sclerosis can mimic the symptoms experienced in manic, hypomanic and depressive episodes [Read More]
Pregnancy
Women predisposed to developing bipolar disorder may experience their first episode during the postnatal period.
[Read more].
What is epidemiology? Epidemiology is the study of the prevalence of disease in different populations and why [Read More].
According to the WHO (World Health Organization), bipolar disorder is the sixth leading cause of disability worldwide [Read More]. Equally prevalent in women and men, an estimated 1% of Canadians will experience bipolar disorder during their lifetime. Women, however, are more likely to seek treatment for the disorder and are hospitalized at higher rates than men [Read More]. The onset of bipolar disorder tends to be between the ages of 15 and 30, with a mean age of 22.5 years old[Read More]. Treatment for bipolar disorder is extremely important as the mortality rate among people with bipolar disorder is 2 to 3 times greater than that of the general population, with higher death rates from suicide, heart problems and other causes. Depressive and mixed manic (both depressive and manic) episodes are the period in which a person is most at risk for committing suicide[Read More].
Psychotherapy
There are many forms of individual and group therapies available to treat depression, including cognitive-behavioural therapy, family-focused therapy and interpersonal therapy.
Cognitive-Behavioural Therapy (CBT): therapy in which the patient learns how to change their negative and harmful thoughts and behaviours.
Family-focused therapy: This type of therapy should be considered when an individual’s depression directly affects the family or the health of a relationship. This type of treatment focuses on the maintenance of clear communication between family members/partners, and educating the family about the illness affecting the individual. This type of therapy can be beneficial because it involves the entire family in helping the family member with bipolar disorder to manage his/her symptoms and adhere to his/her treatment regimen.
Interpersonal therapy: In this type of therapy, the individual learns how to communicate more effectively with others and maintain relationships, as well as keeping to a daily routine that may prevent manic episodes.
Pharmacotherapy
Pharmacotherapy is the treatment of disorders using medication. For the treatment of bipolar disorder, medication is best used in combination with psychotherapy [Read More]. There are three main types of medication used to treat bipolar disorder: mood stabilizers, atypical antipsychotic medication, and antidepressants.
- Mood Stabilizers
- Mood stabilizers are still the first line of medication used to treat bipolar disorder, and it is not uncommon for a patient to continue this treatment for years.
- The most common mood stabilizers are:
- Lithium – often very effective in controlling symptoms of mania and in preventing the return of manic and depressive episodes.
- Anticonvulsants – often used to manage seizures, but are also effective in controlling moods.
- Atypical Antipsychotic Medication
- Atypical antipsychotics are sometimes used to treat bipolar disorder, mostly in combination with other types of medication. They can be used when a person with bipolar disorder experiences psychotic symptoms.
- Antidepressants
- Depending on your symptoms, a doctor may prescribe antidepressants to help treat the depressive episodes of bipolar disorder. Sometimes, antidepressants can trigger episodes of mania/hypomania, which is why they are usually prescribed alongside a mood stabilizing drug.
Psychoeducation
Learn about your disorder, the causes, and treatment options! Join a self-help group or an online forum to share your experiences with others diagnosed with bipolar disorder.
If you think you have bipolar disorder, go see your family doctor, a psychologist or psychiatrist. Ask your family to involve themselves in your treatment program, and adhere to your doctor’s recommendations. Don’t expect an immediate improvement; give yourself time to get better!
Younger people with a low income, recent substance abuse, and a lifetime history of anxiety are at highest risk for developing bipolar disorder [Read More].
Children with a family history of bipolar disorder are 4 to 6 times more likely to develop bipolar disorder than a child with no family history of the disorder [Read More].
What is comorbidity?
Bipolar disorder is highly comorbid with anxiety disorders, panic disorder in particular, and with substance abuse. ADHD has also been found to occur in up to 85% of children with bipolar disorder [Read More].
Adolescents
It can be difficult to determine whether symptoms of bipolar disorder in teenagers are actually due to bipolar disorder or if they are temporary, typical “teenage behaviours”. Symptoms can often look like those of a substance/drug abuse problem, ADHD, or conduct disorder.
Click here to read more about other common symptoms of bipolar disorder in children and adolescents.
Youth-specific resources
National Institute of Mental Health: Bipolar Disorder in Children and Teens
TeenHealth
National Alliance on Mental Illness
HealthLinkBC
Bipolar disorder is a common brain disorder that causes extreme shifts in mood, activity levels and energy. There are three states that are typical of bipolar disorder: mania/hypomania (a ‘high’ state), depression (a ‘low’ state) and a normal state. The onset of bipolar disorder is usually between the ages of 15 and 30. Equally prevalent in women and men, an estimated 1% of Canadians will experience bipolar disorder in their lifetime.
Bipolar disorder can be difficult to detect in teenagers and children due to an overlap between the symptoms of bipolar and those of other common youth disorders. Bipolar disorder is highly comorbid with anxiety disorders (panic disorder in particular), substance abuse, ADHD, and conduct disorder.
Bipolar disorder is a treatable disease that can be overcome or managed using psychotherapy such as cognitive-behavioural therapy, family-focused therapy and interpersonal therapy, and medication such as mood stabilizers, atypical antipsychotic medications, and antidepressants.