Major Depressive Disorder (Depression)
Photo by CraigCloutier
Major depressive disorder, commonly known as depression, is one of Canada’s most prevalent mood disorders and will affect approximately 1 in 10 Canadians during their lifetime. Depression is characterized by feeling sad and depressed consistently for several weeks or months.
Overview
Symptoms
Diagnosis
Causes/Why Me?
Epidemiology
Treatment Approaches
What Can I Do For Myself?
Risk Factors
Comorbidities
Youth Specific Features
Summary
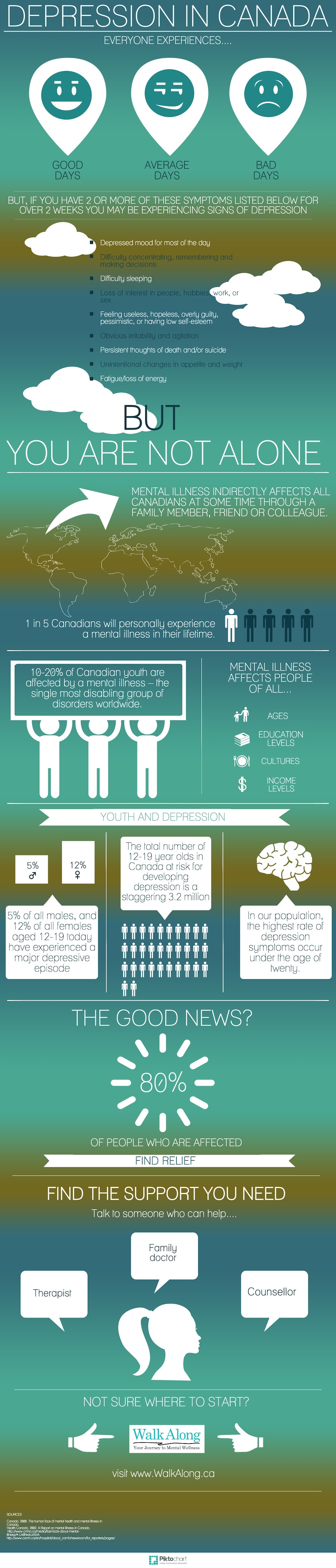
Infographic
Major depressive disorder, commonly known as depression, is one of Canada’s most prevalent mood disorders and will affect approximately 1 in 10 Canadians during their lifetime. The age of onset is between 15 and 30 years of age, and has a lifetime prevalence of 12% in the population.
Depression is characterized by feeling sad and depressed consistently for several weeks or months. People with depression often experience feelings of hopelessness, lethargy (little or no energy), and a lack of pleasure for activities that provided enjoyment in the past. Even small, everyday tasks like getting out of bed and getting dressed become increasingly difficult for someone living with depression. Symptoms of depression include:
- Depressed mood for most of the day
- Difficulty concentrating, remembering and making decisions
- Difficulty sleeping
- Loss of interest in people, hobbies, work, or sex
- Feeling useless, hopeless, overly guilty, pessimistic, or having low self-esteem
- Obvious irritability and agitation
- Persistent thoughts of death and/or suicide
- Unintentional changes in appetite and weight
- Fatigue/loss of energy
To be diagnosed with depression, a person must have experienced a depressed mood and loss of interest in previously enjoyed activities for more than 2 weeks, and show at least 5 of the 9 symptoms listed above.
Click here to view the Diagnostic Criteria for Major Depressive Disorder from the DSM-IV.
Genetic
Some studies suggest that depression is heritable, meaning that a person with a family history of the disorder has a higher chance of developing it.
Biological
Major depressive disorder is largely associated with changes in brain chemistry and function. More recent research has shown that certain diseases (e.g. Parkinson’s, stroke, heart attack, cancer, hormonal changes) can also lead to depression, making recovery more difficult.
Environmental
Experiencing stressful life events (e.g. death of a loved one, financial problems) can also result in an onset of depression. People with low self-esteem, a pessimistic outlook, or those easily prone to stress are also predisposed to developing the disorder.
What is epidemiology? Epidemiology is the study of the prevalence of disease in different populations and why [Read More].
Depression is one of the world’s leading causes of disability, and is more common in women and the divorced or separated. 10% of Canadians will experience major depressive disorder at some point in their life, and the disorder will be chronic in approximately 12% of the cases.
Depression occurs in about 10-25% of women, almost twice as much as in men. Hormonal changes in the body may be the cause of the increased prevalence of depression in women, specifically during the menstrual cycle, during pregnancy and postpartum. Women are also more at risk for depression during a miscarriage, pre-menopause and menopause. Men with depression tend to exhibit more anger and irritability, which often makes it harder to detect [Read More]. Research has shown that the prevalence of major depressive disorder increases with age in single (never-married) men [Read More].
Psychotherapy
There are many forms of individual and group therapies available to treat depression, including cognitive-behavioral therapy, interpersonal therapy, individual psychotherapy, and family/couples therapy.
Cognitive-behavioral therapy: This approach is the most popular form of treatment, and begins by educating the person about depression and how skewed cognition (processing of events, perception, knowledge) is often the cause of the disorder. The emphasis of cognitive-behavioral therapy is to discuss the patient’s thoughts and behaviors associated with depression, and is most effective for people experiencing an average amount of distress from their illness. The treatment is short-term, usually under 24 sessions.
Interpersonal therapy: This is another short-term treatment used for depression. It revolves around maintaining and improving social relationships through improving communication and one’s ability to express emotions.
Family/couples therapy: This type of therapy should be considered when an individual’s depression directly affects the family or the health of a relationship. This type of treatment focuses on the maintenance of clear communication between family members/partners, and educating the family about the illness affecting the individual. This type of therapy beneficial in the sense that it involves the entire family in helping the family member with depression to manage his/her symptoms and adhere to his/her treatment regimen.
Hospitalization
Most depression cases can be treated outside the hospital through therapy and medication. However, sometimes hospitalization may be necessary in cases of severe depression or in which a person is not responding to treatment. A hospital stay may be necessary if a person has attempted suicide or has shown evidence of planning to do so, if the depression has become so debilitating that it has become difficult for the person to take care of themselves, if a new medication has been prescribed and observation is needed, or if a person is receiving treatment that is only available in a hospital (e.g. ECT). A person needing hospitalization should be encouraged to have as much control as they can, i.e. encouraging them to check themselves in voluntarily. Hospitalization tends to be short (24 hours - 4 weeks), usually until prescribed medication or treatment has had an effect. Therapy should be continued after hospitalization to monitor suicidal thoughts, as medication can lead a person to feel more energized and able act upon suicidal thoughts.
Pharmacotherapy
The most common medications prescribed to individuals with depression are known as antidepressants. The most commonly used antidepressants are serotonin re-uptake inhibitors (SSRIs) that work on increasing serotonin levels in the brain. It usually takes between 6-8 weeks of taking the antidepressant to start feeling beneficial effects, but not every medication works for everyone (some may need to try 2-3 different medications to find one that works).
Electroconvulsive therapy (ECT)
ECT is a procedure used to treat severe depression in patients where medication and psychotherapy has had no effect. Patients undergoing ECT are given anaesthesia, and then a mild electric current is passed through the brain for approximately 8 seconds. Due to misrepresentation in the media, ECT is often wrongly viewed as a barbaric treatment by the general public. In reality, ECT is a painless and proven effective short-term treatment for depression [Read More].
Lucy Tallon: How ECT Changed Her Life
Guidelines for ECT use in British Columbia
If you start to recognize the symptoms of depression in yourself, begin by learning more about it. Talk to your doctor about your symptoms and how depression may affect you. Work with your doctor and your friends and family for support to help decide a course of action. There are many online support groups in which individuals with depression can share their experiences and feelings.
Look at our self help tools and track your habits to see patterns in your mood.
Women are more likely to experience major depressive disorder than men, and those with a family history of depression may also be more at risk of developing it. Major stressful life events may also result in the onset of depression.
Depressive symptoms may be the result of another disease with the same symptoms, such as lupus or hypothyroidism, or depression could be a reaction to the development of a serious illness such as cancer or a heart attack. Depression can also be the result of changes in brain chemistry due to an illness such as stroke [Read More]. People with chronic medical illness, low income, and unemployment are also more at risk for developing depression [Read More].
What is comorbidity?
Research shows that depression often occurs with other medical, psychiatric, and substance abuse disorders. Depression has a high comorbidity with anxiety and eating disorders, as well as alcohol and other substance abuse. Clinical studies have shown that 40-65% of patients with myocardial infarctions, 25% of cancer patients, and 10-27% of post-stroke patients suffer from depression [Read More].
In adolescents depression may show through mood swings, sulking, doing badly/getting into trouble at school, showing no interest in activities previously enjoyed, being overly negative and feeling misunderstood. It can sometimes be difficult to tell whether a teenager is going through a certain life stage or has depression [Read More].
Youth-specific resources
Students Against Depression
Major Depressive Disorder, more commonly known as Depression, is one of Canada’s most prevalent mental disorders and will affect 1 in 10 Canadians during their lifetime. Depression is characterized as feeling sad and depressed consistently for several weeks or months. People with depression often experience feelings of hopelessness, lethargy (little or no energy), and a lack of pleasure for activities that provided enjoyment in the past.
Depression expresses itself differently between men, women, and children, and tends to be more difficult to detect in men and children. Women are more likely to experience major depressive disorder than men, and those with a family history of depression may also be more at risk of developing it. Major stressful life events may also result in the onset of depression. Depressive symptoms may be the result of another disease with the same symptoms, such as lupus or hypothyroidism, or depression could be a reaction to the development of a serious illness such as cancer or a heart attack. Depression can also be the result of changes in brain chemistry due to an illness such as stroke.
Psychotherapy, hospitalization and pharmacotherapy are three different treatment approaches. Cognitive-behavioral therapy is the most popular form of psychotherapy, and antidepressants are the most widely used form of medication. Research shows that depression often occurs with other medical, psychiatric and substance abuse disorders. Depression has a high comorbidity with anxiety and eating disorders, as well as alcohol and other substance abuse.