Obsessive-Compulsive Disorder (OCD)
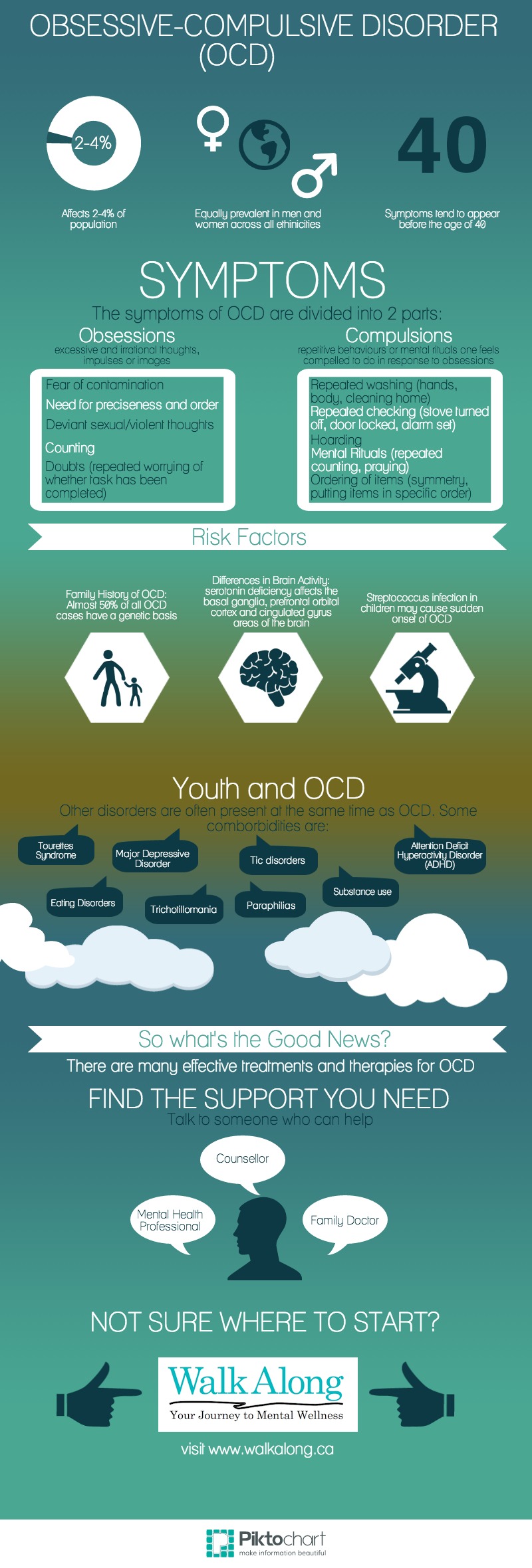
Obsessive Compulsive Disorder (OCD) is a psychological disorder characterized by obsessive and compulsive behaviours that cause a person great distress and affect the normal functioning of everyday life. Symptoms consist of obsessions (recurring and persistent thoughts) and compulsions (repetitive behaviours or mental rituals) that together cause the person great distress, are time-consuming, and affects the normal functioning of everyday life. OCD is the fourth most frequently occurring psychological disorder and is equally prevalent in men and women.
Overview
Symptoms
Diagnosis
Causes/Why Me?
Epidemiology
Treatment Approaches
What Can I Do For Myself?
Risk Factors
Comorbidities
Youth Specific Features
Summary
The symptoms of OCD are divided into two parts: Obsessions and Compulsions.
Obsessions
Obsessions may include recurring and persistent thoughts, impulses, or images that are more than worries about real-life issues. People with OCD will recognize that these obsessions are self-induced, excessive, and irrational. As a result, the person may attempt to supress or reject these thoughts.
Common obsessions [full list] may include:
- Fear of contamination
- Need for preciseness and order
- Counting
- Deviant sexual or violent thoughts
- Doubts (such as repeatedly worrying whether a certain task has been completed).
Compulsions
Compulsions are repetitive observable behaviours or mental rituals that a person feels compelled to do in response to the obsession in an attempt to neutralise or suppress feelings of anxiety. Such behaviours will clearly not have a suppressive effect on the obsessions, and often people with OCD will recognize the uselessness of their behaviour (with the exception of children) but feel powerless to stop themselves. Performing these rituals often provides temporary relief of the anxiety produced by OCD.
Common compulsions [full list] may include:
- Repeated washing (of hands, body, cleaning one’s home, etc)
- Repeated checking (whether lights are on, stove is turned off, etc)
- Hoarding
- Mental rituals (repeated counting, praying, etc)
- Ordering of items (e.g. putting things in specific order or symmetry).
To be diagnosed with OCD, a patient must be experiencing symptoms to an extent that causes him or her great distress, are time-consuming, and affect the normal functioning of his or her daily life. Obsessiveness or compulsiveness characteristic of OCD must not be confused with obsessive-compulsive personality disorder, and the symptoms must not be the result of another Axis I disorder, a pre-existing medical condition, or substance abuse [Read More].
Click here for the DSM-IV Diagnostic Criteria for Obsessive Compulsive Disorder
Symptoms usually begin to appear before the age of 40. OCD can be caused by a combination of psychological, biological, and genetic factors.
Genetic factors
Almost 50% of all OCD cases have a genetic basis (runs in the family). A person with an immediate family member with OCD are at higher risk of developing OCD themselves as opposed to someone with no family history of OCD. Some research has shown that families with a history of Tourette’s syndrome are also at higher risk for developing OCD, suggesting that there is a genetic link between these two disorders [Read More].
Biological factors
Studies done on changes in brain activity have shown that people with OCD have more activity in the basal ganglia, prefrontal orbital cortex and cingulated gyrus areas of the brain. These areas are all affected by serotonin, a chemical messenger that appears to be lacking in people with OCD [Read More]. One uncommon form of OCD can begin after Streptococcus, a bacterial infection [Read More].
Psychological factors
Two of the main theories that have been introduced to explain OCD are the Behavioural theory and the Cognitive theory.
- Behavioural theory: this theory argues that people with OCD with a fear of certain objects or situations learn to avoid their fear or perform rituals (compulsions) in order to reduce the anxiety associated with that specific object or situation.
- Cognitive theory: this theory argues that people with OCD misinterpret their thoughts (obsessions), and react as if these thoughts are harmful. For example, a person with OCD who has persistent thoughts about harming their family might believe that he/she is a threat to them.
What is epidemiology? Epidemiology is the study of the prevalence of disease in different populations and why [Read More].
OCD is the fourth most frequently occurring psychological disorder and in 2% - 4% of the population, it is chronic. Men and women adults of any ethnicity are equally as likely to develop the disorder, and symptoms usually begin to appear before the age of 40. However, early onset before or during adolescence most frequently occurs among males. OCD is generally persistent and long lasting (more than three months, and sometimes chronic). OCD is often underdiagnosed or unrecognized, the average time between onset and correct diagnosis being seventeen years [Read More].
Pharmacotherapy
Pharmacotherapy is the treatment of a disorder using medication. Research has shown that people with OCD benefit from medicines that increase serotonin levels, and the primary medications used are known as serotonin reuptake inhibitors (SRIs). In some cases where a person does not benefit from an SRI, a different antidepressant or an additional (secondary) medication may be prescribed.
- Serotonin reuptake inhibitors (SRIs): SRIs are antidepressants, and are therefore also used to treat depression. 75% of people who are prescribed SRIs to treat their OCD experience a reduction in their symptoms.
- Other antidepressants: also affect serotonin levels, but in a different way than SRIs.
- Secondary medications: anxiety-relieving drugs (e.g. benzodiazephines), antipsychotics (e.g. haloperidol), mood stabilizers (e.g. lithium), and herbal treatments (sedating and non-sedating) [Read More].
Cognitive-Behavioural Therapy (CBT)
What is CBT? Cognitive behaviour therapy is a form of treatment which teaches a person with OCD to challenge and re-evaluate his/her obsessions, and to point out and examine any potential fearful thoughts about the consequences of not partaking in compulsive behaviours.
CBT also involves exposure and response prevention (ERP) which involves controlled exposure to objects or situations that trigger obsessions (exposure) and learning how to resist compulsions that arise from the anxiety-producing obsession (response prevention) [Read More].
Psychoeducation
Psychoeducation is where you educate yourself about a certain disorder. Learning about your situation can help you understand your illness and work towards making changes and seeking outside help.
If you think you have OCD, go see your family doctor, a psychologist or psychiatrist. Ask your family to involve themselves in your treatment program, and adhere to your doctor’s recommendations. Don’t expect an immediate improvement; give yourself time to get better!
People with a family history of OCD or who live with people who have OCD are more likely to experience it themselves. Among children with OCD, 18% - 30% of their relatives also exhibited obsessive-compulsive symptoms [Read More]. Undergoing periods of high emotional stress may cause obsessive-compulsive patterns to appear. Streptococcus infection in children may also cause a sudden onset of OCD [Read More].
What is comorbidity?
OCD often occurs with other Axis I disorders such as body dysmorphic disorder, hypochondriasis, substance use disorder, paraphilia, major depressive disorder, trichotillomania, tic disorders and eating disorders. In children, OCD can also be comorbid with Tourette syndrome, ADHD, and separation anxiety.
Comorbidity with depression increases significantly from childhood to adolescence, and comorbidity with Tourette syndrome is more common in children than in adults. ADHD is also comorbid with OCD in children, with a higher prevalence seen in males. Obsessions of separation and harm involving family members are common, with a higher occurrence of comorbidity with separation anxiety [Read More].
Youth-specific resources
TeenMentalHealth
AnxietyBC
KidsHealth
Anxiety and Depression Association of America: Personal Stories - OCD
Beyond OCD: Personal Stories
International OCD Foundation: Personal Stories
Obsessive Compulsive Disorder (OCD) is a type of anxiety disorder characterised by obsessive and compulsive behaviours. An adult experiencing OCD will understand that his or her behaviour is not normal, but feels incapable of stopping the behaviour. When OCD occurs among youth (around the ages of 7-13), it normally affects boys, whereas adult onset affects men and women equally. Current research suggests that OCD is largely a result of genetics, meaning that a person who has a close relative with the disorder is more likely to develop it. However, OCD can also be the result of environmental factors such as surrounding oneself with people who exhibit OCD-related symptoms. OCD commonly occurs alongside other Axis 1 disorders such as other anxiety or mood disorders. Treatment appears to be most effective when it is a combination of psychotherapy (Cognitive Behavioural Therapy) and pharmacotherapy (medication such as SRIs). If you think you have OCD, go see your family doctor, a psychologist or psychiatrist. Ask your family to involve themselves in your treatment program, and adhere to your doctor’s recommendations. Don’t expect an immediate improvement; give yourself time to get better!