Panic Disorder (PD)
Panic disorder (PD) is a psychological disorder characterised by panic attacks and a constant fear of experiencing another panic attack in the future. PD affects approximately 2 million Canadians, and 4% of Canadians will experience PD during their lifetime.
Overview
Symptoms
Diagnosis
Causes/Why Me?
Epidemiology
Treatment Approaches
What Can I Do For Myself?
Comorbidities
Youth Specific Features
Personal Stories
Summary
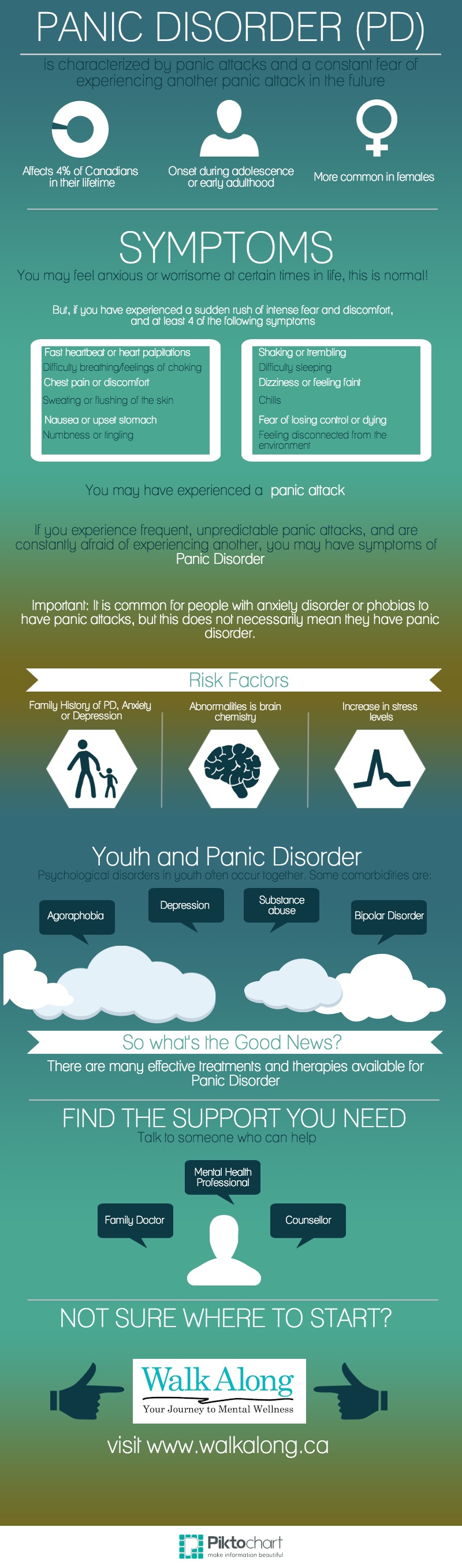
Infographic
Panic disorder (PD) is a psychological disorder characterised by panic attacks and a constant fear of experiencing another panic attack in the future. A panic attack is characterized by sudden arousal of the autonomic nervous system, resulting in intense feelings of fear and anxiety and a number of physical symptoms such as a fast heartbeat, difficulty breathing and dizziness. PD can be diagnosed with or without agoraphobia. PD affects approximately 2 million Canadians, and 4% of Canadians will experience PD during their lifetime. Onset occurs most often during adolescence or young adulthood.
Panic disorder (PD) is a psychological disorder characterised by panic attacks and a constant fear of experiencing another panic attack in the future. A panic attack is identified by sudden bursts of arousal of the autonomic nervous system (parts of the body which react involuntarily and reflexively to stimuli, such as muscles, eyes, the heart and the stomach). Panic attacks are experienced as a sudden rush of intense fear and discomfort, and include at least four of the following symptoms:
- Fast heartbeat or heart palpitations
- Difficulty breathing or a feeling of choking
- Chest pain or discomfort
- Sweating or flushing of the skin
- Nausea or upset stomach
- Numbness or tingling
- Shaking or trembling
- Difficulty sleeping
- Chills
- Dizziness or feeling faint
- Feeling disconnected from the environment
- Fear of losing control
- Fear of dying
Attacks tend to peak at 10 minutes, and people experiencing them feel as if they have a serious medical problem requiring emergency treatment (e.g. a heart attack). Panic attacks are often unpredictable and unrelated to any specific trigger, which can cause a person with panic disorder to develop agoraphobia, which affects a third of people with PD.
Panic attacks may be experienced by people who do not have Panic Disorder. A person is diagnosed with PD if panic attacks occur frequently, spontaneously (without the occurrence of a panic-inducing event), and are followed by anxiety over having another panic attack for at least thirty days.
Symptoms must not be the result of another medical condition (e.g. anemia, thyroid disorder).
Click here for the DSM-IV Diagnostic Criteria for Panic Disorder with Agoraphobia
Click here for the DSM-IV Diagnostic Criteria for Panic Disorder without Agoraphobia
Research suggests that PD is the result of both genetic and environmental factors. Heritability (the chance of developing the disorder when you have an immediate family member with the disorder) is suggested to be 40%. Having a family history of anxiety or depression may also increase the risk of developing PD. Individuals with the disorder are also shown to have abnormalities in brain chemistry and activity. The onset of PD is often preceded by a period of high stress, or the anticipation of a stressful event [Read More].
What is epidemiology? Epidemiology is the study of the prevalence of disease in different populations and why [Read More].
PD affects approximately 2 million Canadians, and 4% of Canadians will experience PD during their lifetime. Onset occurs most often during adolescence or young adulthood. Women and previously married people have a higher chance of developing PD, and those over 60 years of age appear to be at lower risk [Read More].
Psychoeducation
Psychoeducation is where you educate yourself about a certain disorder. Learning about PD can help you feel more in control of your situation and reduce some of the stress that comes with it.
Cognitive Behavioral Therapy (CBT)
What is CBT? CBT is a proven-to-work treatment that focuses on the belief that your thoughts (cognitive) influence the way you act (behavioural), and works on changing the way you think and act. Your way of thinking (cognitive) can trigger or stimulate panic attacks and agoraphobia, and changing the way you perceive situations (through CBT treatment) can help manage and prevent panic attacks. The behavioural aspect of CBT involves changing harmful and/or non-helpful behaviours, which can be useful for people with agoraphobia who avoid certain places/situations [Read More]. CBT also involves exposure to places and/or situations in which you fear having a panic attack (in-vivo exposure) and practicing realistic thinking by challenging negative thoughts (cognitive restructuring). [Read More].
Pharmacotherapy
Antidepressants and anti-anxiety medications are the usual medication prescribed to people with panic disorder. Different people benefit from different forms of treatment (e.g. certain people do not benefit from cognitive-behavioural therapy and some only need cognitive-behavioural therapy to treat their PD). The right combination of treatment (medication and/or psychotherapy) brings relief to 70-90% of patients with PD. If a person experiencing panic disorder is also abusing drugs or alcohol, their substance abuse should be treated as well. People with PD often turn to drugs or alcohol in an attempt to treat their anxiety, when in reality these substances can trigger panic attacks or result in dependency [Read More].
Psychoeducation
Learn about your disorder, the causes, and treatment options! Join a self-help group or an online forum to share your experiences with others diagnosed with PD.
If you think you have PD, go see your family doctor, a psychologist or psychiatrist. Ask your family to involve themselves in your treatment program, and adhere to your doctor’s recommendations. Don’t expect an immediate improvement; give yourself time to get better!
AnxietyBC Self-Help Guide
MoodJuice Self-Help Guide
What is comorbidity?
PD rarely exists without another psychological condition. Agoraphobia, major depressive disorder, bipolar disorder, and substance abuse often exist with and worsen the disorder. Cardiovascular, respiratory (e.g. asthma), and otological (ear) disorders can also occur with PD. Depression is present in 50-65% of people with PD [Read More].
Some research suggests that daily smoking is associated with an increased risk for a first panic attack and this risk is higher in active (as opposed to past) smokers. Non-smokers with lung disease have also been identified has having a higher risk for experiencing panic attacks [Read More].
Adolescents (as opposed to children) are able to describe their psychological and physical symptoms and the experience of having a panic attack. An adolescent with panic disorder may avoid places where they think they will have a panic attack, worry persistently about future panic attacks, fear of dying, low self-esteem, isolation from friends, reluctance to participate in activities and experimentation with drugs. Panic disorder tends to develop during adolescence, but may also begin in childhood [Read More].
Youth-specific resources
TeenMentalHealth
Anxiety in Teens
Anxiety and Depression Association of America – Personal Stories
Panic disorder (PD) is characterised by panic attacks and a constant fear of experiencing another panic attack in the future. A panic attack is identified by the sudden bursts of arousal of the autonomic nervous system (parts of the body which react involuntarily and reflexively to stimuli, such as muscles, eyes, the heart and the stomach). Panic attacks are experienced as a sudden rush of intense fear and physical as well as psychological discomfort. Panic attacks tend to peak at 10 minutes, are often unpredictable and unrelated to any specific trigger, which can cause a person with panic disorder to develop agoraphobia. Treatment options include cognitive behavioural therapy and medication. Panic disorder rarely exists by itself, and is often comorbid with depression, bipolar disorder and substance abuse. Children exhibit slightly different symptoms of panic disorder as they can often not clearly voice their experience with panic attacks, but adolescents tend to show the same symptoms as adults. Panic disorder affects approximately 2 million Canadians and tends to develop during adolescence, but may also start in childhood.